Let's talk about the things I don't talk about. The things I carry with me each day—silently—as I go about my business living as close to a normal life as I can. The things that weigh on my shoulders—things that I didn't even know were there—until they've been lifted.
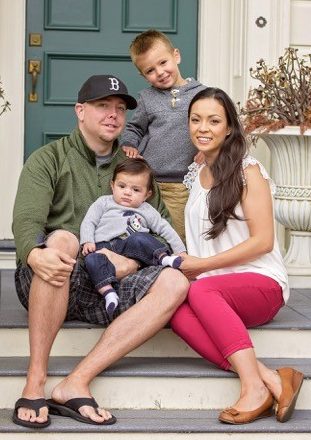
Hi. My name is Melissa. I’m 35. I have two amazing baby boys who are 3.5 years old and 9.5 month old. I’m also married to Mr. Wonderful. A month and a half after I married Mr. Wonderful, I was diagnosed with stage IIA breast cancer. I was 29 years old. I opted for a double mastectomy and four rounds of chemotherapy. I passed my “five year mark” —the point at which your chance of recurrence statistically goes down significantly—in May 2015 without incident. I was 2 months pregnant at the time with our littlest. In January 2016, five weeks postpartum, I went in for an MRI of my neck. There was a lingering “pregnancy pain” that just wasn’t going away. On January 21 I got a call from my PCP who ordered the scan. She said the radiologist wanted me back in to rescan, this time with contrast. There was something “not right.” I went in the next day. I cried on the MRI table and had to pause the scan. I knew. I knew in my bones what was happening. That night I received another call from my PCP to discuss results.
On January 22, 2016 I was diagnosed with metastatic breast cancer a.k.a. stage IV. The pain in my neck was from a tumor that had eaten away half of the left side of my C3 vertebrae. I was 2 months way from turning 35. I hadn’t even had my 6 week postpartum check-up yet.
After the MRI, we went through the whirlwind that is diagnosis and immediate surgeries and treatments to stabilize my neck and get a fuller picture of “the spread.” In addition to my C3, there were metastases to the cricoid cartilage that had narrowed my airway by 40% and required a tracheostomy to be put in place as well as a 4 cm conglomerate mass of nodes and nodules in my right lung, additional spots in various bones throughout the body as well as 3 spots in the brain. Radiation therapy has been my friend and has saved me from a fractured hip and hip replacement and from suffocation and paralysis. I’ve said goodbye to my ovaries, as well as any chance of additional children, am taking a $10,000 a month breakthrough medication ($476 per pill), a daily aromatase inhibitor, a $5,000 once monthly injection for my bones and a about 12-14 supplements, two times a day. In nine months, I’ve had two surgeries, three PET CTs, three individual CTs, 10 or so MRIs, and 46 sessions of radiation … give or take … and I don’t even want to count how many times I’ve had my blood drawn or an IV set.
And so here we are today, 9 months later from that existence-altering event … in a window of calm between scans. I’m 35, and I’m slowly learning to cope. Every morning I wake up and sleep the night before was OK. I often wake up in the middle of the night. Sometimes it's just because, sometimes it's because Nicholas wakes ... other times it's because Camden is standing silently next to the bed, staring at me, and his presence alone startles me awake. Yeah, those aren't the fun wake-ups. Those are the creepy, send your heart racing, why are you standing there in the dark watching me wake-ups. Always fun. But when I wake in the morning, I'm usually only semi-rested, and I'm creaky. I put my feet down, and they hurt. They're stiff. I reach for my glasses and my hands are stiff. They hurt also from the lack of movement all night. I can’t make a fist with my right hand because experiencing trigger finger with my middle finger from who knows what. It just locks up in the bent position if I try, and then it "pops" semi-painfully when I open my fist all the way. For the most part, these aches in my hands and feet start to go away as I start to move. But there's always some level of ache to them, and I'm constantly stretching my fingers and toes throughout the day.
The next thing I usually notice when I wake up is a pain in my spine. The location varies, but it's usually always a sharp ache somewhere along my spine. Some days it's worse ... some days it's better ... but most days it's always there. It started shortly after my oophorectomy, and I can only thus attribute it to the severe withdraw of estrogen. In addition to these usual suspects, most often there's something new each day. An ache, throb, pain, twitch, creak, pop, stab, pulse, twang, knot, crack, pressure, weight ... you name it ... somewhere else in my body. Big deal right? Everyone has regular aches and pains. I get it. And it's not the creakiness and errant odd feeling that bother me so much as it is what it does to me mentally. Being in treatment causes me to be hyper aware of my physical state. As someone who was already hyper aware of her physical state in general ... this takes it to a whole new level. Each "thing" I feel, I carry with it a monitoring. When did I first notice it? Is it getting better or worse? How long has it been? Do I need to bring it up to my doctor? Is it something ... no—it’s nothing ... or is it something? It's a constant assessment of my physical state day to day, hour to hour, minute to minute ... over and over again ... worrying if it's progression ... if things are just running rampant inside during this period of in-between scans. And then, when I don’t feel anything, I wonder why and worry even more about why I can’t feel anything. It gets exhausting. But I keep going, every day assessing quietly and taking a mental catalog as each day goes on. And that’s just below the neck activity. Layer on top of that, the situation with the brain. Every headache, every ANYthing I feel in or around my head—or anything anywhere else in my body—is there something going on in my brain that's causing this? Is it a dehydration headache or something more? Am I going to go down in a seizure right here and now? UGH.
In addition to this physical assessment, there's the daily fatigue. Having low counts in your blood causes fatigue. I'm tired. I usually make it to just past 9 p.m. before I'm crawling in bed myself and am passed out shortly thereafter. If I stop moving, I will fall asleep. I'm sure of it. So I keep busy as much as possible, either physically or mentally. I just keep going. I'm up with the boys at 7 a.m. usually and in bed shortly after the oldest goes down at 9 p.m. Most of the time I've got energy enough to keep going full steam all day. But some days, a big outing is enough to slow me down, and I end up wanting to nap with the boys when we get home.
So there's the physical part, the mental part of the physical part, the mental part of the mental part, and the fatigue. And then there's Fear. Is eating "this" feeding the cancer? Should I be doing more? What if what I'm doing now is making things worse? How long will what I'm doing work? Will I have to have IV chemo again ... or worse? Any regular conversation that talks about the future: future plans, future milestones for the boys, future vacations, future anything ... it’s all haunted by the fear. Will I be around to see these plans come to fruition? How long am going to feel "good?" Will I be around to see my boys start school ... start middle school ... high school? Do I dare to dream ... dare to hope ... that I get to see at least one of my sons get married? The fear isn't always front and center ... no. It's most often a passing thought ... an errant question that runs through my head quickly in the moment ... a hypothetical visualization of who and how I might be, or who and how I fear I might be. A shadow that follows my thoughts. It's there when I look at Nicholas and wonder ... does he look so much like me because I'm not going to be around much longer? Is he my mini-me for a reason? Or is it purely just genetics. And if it's not just genetics, and if something does happen to me, will Mike, in time, be able to look at his sons without significant pain in his heart? And my boys: I can’t even touch those thoughts about them growing up without me.
I wonder about this and many, many other things. And I worry every day. But I won't go much farther down this path. These are things I don't talk about for a reason. There are things that come with the territory unfortunately, and, well, there's no use dwelling on them. No use losing the present to fear and worry. So I let go of what I can and shove that which I can't, down into the depths, until I'm able to let it go.
These last few weeks have been seriously trying. The "questionable leptomeningeal enhancement" on my brain MRI in August had us all in a serious frenzy. The suggestion of it at my initial neuro appointment injured my spirit in so many ways. It brought Fear front and center. But thankfully, my rainwater cerebral spinal fluid (CSF) came back 100% normal. My neuro onc at this most recent appointment said it would be one thing if it was "mostly" normal, with some things slightly abnormal, but mine coming back 100% normal was a good thing. He reviewed my follow-up brain MRI, and Mike and I stood anxiously over his shoulder. I'm watching the scans and watching his eyes and expression as he's reviewing, trying to get a read on his reaction to what he's seeing. And then he pushed back from the computer screen (he sits about eight inches away from the screen when he reviews images), takes his glasses off and says, "I don't see anything here to get excited about." And then suddenly I feel SO MUCH LIGHTER. I breathe. And I tremble with relief. I grab Mike's arm. I just grab him. And I get back to myself and start to ask questions. What about the questionable LMD spot, left temporal left cerebellum region? You don't see that? He puts his glasses back on, scoots up to the computer and looks again. He swaps out views, scrolls, swaps out more views, scrolls some more. No he says. And I don't remember much detail after that.
Overall, he concluded that things look normal for me. Two spots of the three spots are identifiable, but smaller and stable. One spot he can't even find anymore. The questionable LMD area is not there. "Most likely a vein" the radiologist's report said. So we breathe finally. And we are thankful. So very, very thankful.
I re-scan in two months, which is back in sequence with my regular timing for my 3 month interval PET CT and brain MRI. I started cycle 7 of Ibrance with Letrozole, received my monthly injection in the belly, all with sincere hopes that it continues to work much longer (aka forever). I started back at work this month as well, which I'm excited about, to get back into some normal life again.
And above all else—every day, every moment—with every breath, I give sincere thanks for waking up each day and I dare to hope, just a little bit more. Each time I hug my babies or hold Mike's hand, I dare to hope that I get the chance to grow old.
Metastatic Breast Cancer Awareness Week
Until 2009, metastatic breast cancer was not often mentioned during Breast Cancer Awareness Month. Nine metastatic breast cancer patients, including one of YSC’s early members, Randi Rosenberg, traveled to Washington, D.C. to change that. Their efforts resulted in the passing of a unanimous resolution by Congress declaring October 13 as Metastatic Breast Cancer Awareness Day.
Metastatic (or stage IV) breast cancer is when cancer has left the breast and surrounding local area and moved to other parts of the body, such as the liver, lungs, bones or brain. Once it has metastasized, there is no cure for breast cancer. The disease turns into a chronic condition with the goal to contain it for as long as possible. Every year, more than 1,000 women under age 40 die from breast cancer. That’s why we’re dedicating this entire week to raising awareness of metastatic breast cancer and advocating for more research on metastatic disease by featuring women who know firsthand what life is like living with stage IV.
Join us every day this week for new blog posts from young women living with metastatic breast cancer or experts on metastatic research.
Please sign our #12Ktoomany petition now.
Our goal is to collect 12,000 signatures to represent the 12,000 young women who will be diagnosed under 40 this year in the US. We’re urging the new President to focus at least 50% of research dollars to examine metastasis in young women, including how to cure metastasis and how to prevent it.
Let's dare to hope together with Melissa, and other young women facing metastatic breast cancer, who deserve the chance to grow old.