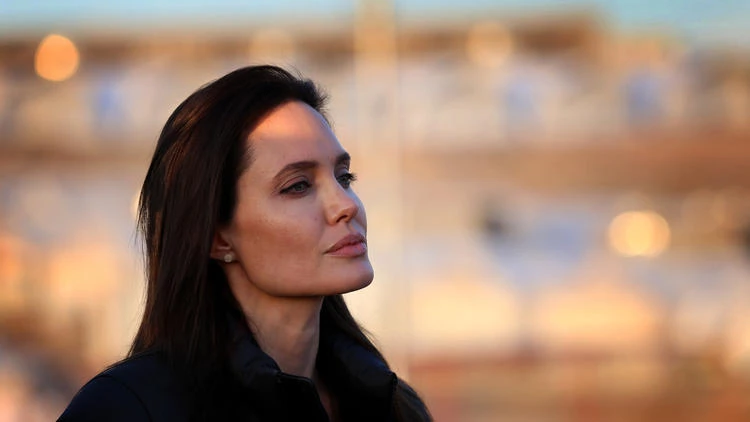
All of us have heard the news about Angelina Jolie Pitt choosing to have her ovaries and fallopian tubes removed as a means of preventing ovarian cancer.
Angelina Jolie's message was “choose what's right for you,” and the experts agree. She says, “It is not easy to make these decisions. But it is possible to take control and tackle head-on any health issue. You can seek advice, learn about the options and make choices that are right for you. Knowledge is power.”
I couldn’t agree more. YSC strongly believes and encourages young women to know their bodies, advocate for their own health and persist in asking questions if something doesn’t seem right. It is critical that young women make decisions based on the most current, evidence-based information available; ask questions and feel empowered to get a second opinion!
I applaud Angelina’s frankness and honesty in sparking a discussion in the media that must continue to spread around the world…young women CAN and DO get breast cancer!
Something else I appreciated was that Angelina highlighted the importance and impact of this experience on her co-survivor, Brad Pitt. This truly acknowledges the importance of co-survivors in our journeys! My favorite quote from the Op-ed is, “The beautiful thing about such moments in life is that there is so much clarity. You know what you live for and what matters. It is polarizing, and it is peaceful.” Every young woman diagnosed with breast cancer and her co-survivor knows EXACTLY what she means.
To gain a deeper and more personal perspective than mine, YSC spoke with Dr. Corinne Menn. Dr. Menn is a board-certified gynecologist and a young breast cancer survivor. She was diagnosed at age 28, only six weeks after losing her mother to ovarian cancer.
Although Dr. Menn’s initial test came back negative for BRCA 1 and BRCA 2 mutations, she chose to undergo a bilateral mastectomy to prevent the future recurrence of breast cancer. Several years later, she had a prophylactic bilateral salpingo-oophrectomy (BSO) - the same procedure Angelina underwent - to prevent ovarian cancer.
YSC: Tell us your thoughts after reading the Op-ed by Angelina Jolie Pitt and subsequent news coverage. Is this procedure “news” and do you think it should cause concern for healthy young women?
Dr. Menn: I’m glad to see that Angelina brings light to this women’s health issue. I particularly like that she notes that “health choices are a part of life not to be feared.” It’s important for patients to be aware of their health choices and not to be afraid of them.
Those who are at-risk are afraid to know whether they are BRCA positive or not, even if they are breast cancer survivors. The main fear I hear is about the physical implications of knowing. The belief that, “if I’m BRCA positive, I must have surgery,” is false. There are many choices that come along with being high risk. You must weigh your options and make the choice that is right for you and your family. The more information you have, the more empowered you will be.
YSC: How do women know if they should or shouldn’t be tested for BRCA?
Dr. Menn: There are excellent guidelines and risk assessment questionnaires that help clinicians decide who should receive BRCA testing. In the past, the threshold was higher and testing wasn’t routinely discussed or offered to patients. Doctors shouldn’t test everyone, but everyone should have a conversation about their family history with their doctors at least every few years, or as their family history changes. One thing to note is that if patients had the test before 2012, it may not have been screened for a mutation in a large rearrangement of the gene, also know as the (BART) test, which accounts for a small percentage of mutation problems in BRCA-positive patients.
My mother died of ovarian cancer at 54, only six weeks before I was diagnosed with breast cancer. After my chemotherapy treatments were done, I was tested for BRCA. I was negative, but it didn’t sit right with me, given my family history. I decided to pursue a bilateral mastectomy and treat myself as being BRCA positive.
Through my practice, I became more knowledgeable about BRCA and asked to add the BART sequence as a part of my testing. Guess what? It turns out I am BRCA 2 positive. Not only am I positive, but my brother, maternal aunt, and cousin are all BRCA 2 positive, too. It is amazing how this one piece of information has impacted my family.
I hear stories all the time from patients who were either not offered the test or were tested prior to 2012, when the comprehensive gene analysis became standard. I have made it my practice to ask women when they were tested and to follow up on the BART test if it was not included.
YSC: Please share with us what considerations and options you had to think about before choosing to undergo the BSO procedure at age 34.
Dr. Menn: It was a hard and emotional decision because it means closing the door on becoming pregnant and because, particularly as a gynecologist, I knew what early menopause meant for me. On the other hand, I had survived cancer once and experienced the untimely death of my mother. I wanted to be there for my children and husband, and ultimately the benefits of protecting myself from the recurrence of breast cancer and ovarian cancer outweighed the downside of early menopause and everything that comes along with it. Even if you are not BRCA positive, it is very likely insurance will cover the BSO procedure, if it is being done appropriately based on genetic factors and risk factors.
YSC: What are some things to consider concerning family planning when deciding if/when to have the procedure? Should someone be BRCA positive or be high risk due to their family history?
Dr. Menn: Many people don’t know this, but emerging studies show that with the BRCA 1 gene, your risk of ovarian cancer comes at an earlier age. We recommend that if you are deciding to undergo the BSO procedure and you’re BRCA 1 positive, that you have it done once you are done childbearing or before the age of 35, whichever comes first.
For those testing positive for BRCA 2, the risk of ovarian cancer comes later in life and you could wait until the age of 40 to undergo a BSO. There is also emerging evidence that ovarian cancer starts in the fallopian tubes. Therefore, some patients are choosing to do their BSO in a two-step process by removing their fallopian tubes first and keeping their ovaries until fertility is not an issue.
There are many options to consider, and women don’t need to make a decision right away. Once a woman decides to have the surgery, there are many health risks to consider. Make sure to push the clinicians to give the appropriate options and treatments that must be considered when removing one’s ovaries, namely for treating early menopause.
YSC: Could you tell us more about the side effects of early menopause? Is there anything breast cancer survivors can do to alleviate them?
Dr. Menn: Immediate surgical menopause comes with many side effects. I see many patients who are not aware of treatments for menopause. Patients need to ask their doctors about how they will manage the side effects before having any procedure done. Often, doctors will tell their patients to “just deal with it; it’s menopause,” which is totally unacceptable.
Some side effects include insomnia, weight gain, sexual dysfunction, vaginal dryness and mood changes. The approach to menopause varies widely, but there are many non-hormonal things like lifestyle changes and holistic options that can work. It depends on the patient, but I recommend many non-hormonal treatments for breast cancer survivors.
Valerian root is really helpful in treating insomnia. There are great herbal formulations available for hot flashes. I recommend a local vaginal estrogen, even in breast cancer survivors, to help with vaginal dryness and sexual dysfunction. Coconut oil is also a great natural option. For those who have never been diagnosed with breast cancer, there are many options such as the estrogen patch, progestin IUD and oral progesterone.
YSC: As a young breast cancer survivor, please share your experiences with YSC.
Dr. Menn: I found Young Survival Coalition (YSC) when I was diagnosed with breast cancer at the age of 28 and it was my absolute lifeline. YSC gave me hope and made me feel like I was not alone. YSC immediately connected me with other survivors who had already gone through treatment, and their support was invaluable.
I remember going in to receive chemo and being the only young person in the waiting room. I felt like everyone was looking at me and feeling sorry for me. It was very isolating. When I found YSC, I no longer felt alone. I have met so many wonderful young women as a result, some of whom are now lifelong friends.
The silver lining to breast cancer has been my involvement in YSC— from riding the Tour de Pink, to attending In Living Pink, to now leading the Westchester County Face 2 Face group. Breast cancer and being BRCA positive has led me to dedicate much of my practice to helping other survivors deal with their unique female health issues.
Thank you so much for sharing, Dr. Menn. I am certain many women out there will benefit from your story and expertise.
Find out more information on the BRCA gene.
If you or someone you know is at high risk for breast or ovarian cancer but has not been diagnosed with it, learn more from our partner, Bright Pink.
You may also wish to learn more about Dr. Menn.