Today, the American Cancer Society (ACS) revised its guidelines on screening mammography and clinical breast exams (CBEs) in the Journal of the American Medical Association (JAMA). These new guidelines state that, in women of average breast cancer risk, annual screening mammography should start at age 45 and that CBEs should not be performed by physicians on women of any age. For women ages 40-44, the guidelines state that they should have the “opportunity” to begin annual mammography screening. Prior to this October publication, ACS recommended annual mammograms starting at age 40 and CBEs every three years for women in their 20s and 30s, with annual CBEs to begin at age 40.
As the leading voice for young women affected by breast cancer, Young Survival Coalition (YSC) has released a response on these new guidelines. We carefully reviewed all available research when taking a stance on these issues. We believe that better tools are urgently needed to screen, diagnose, detect and monitor for breast cancer in younger women. You can read our full response here.
Let’s break it down a bit further…
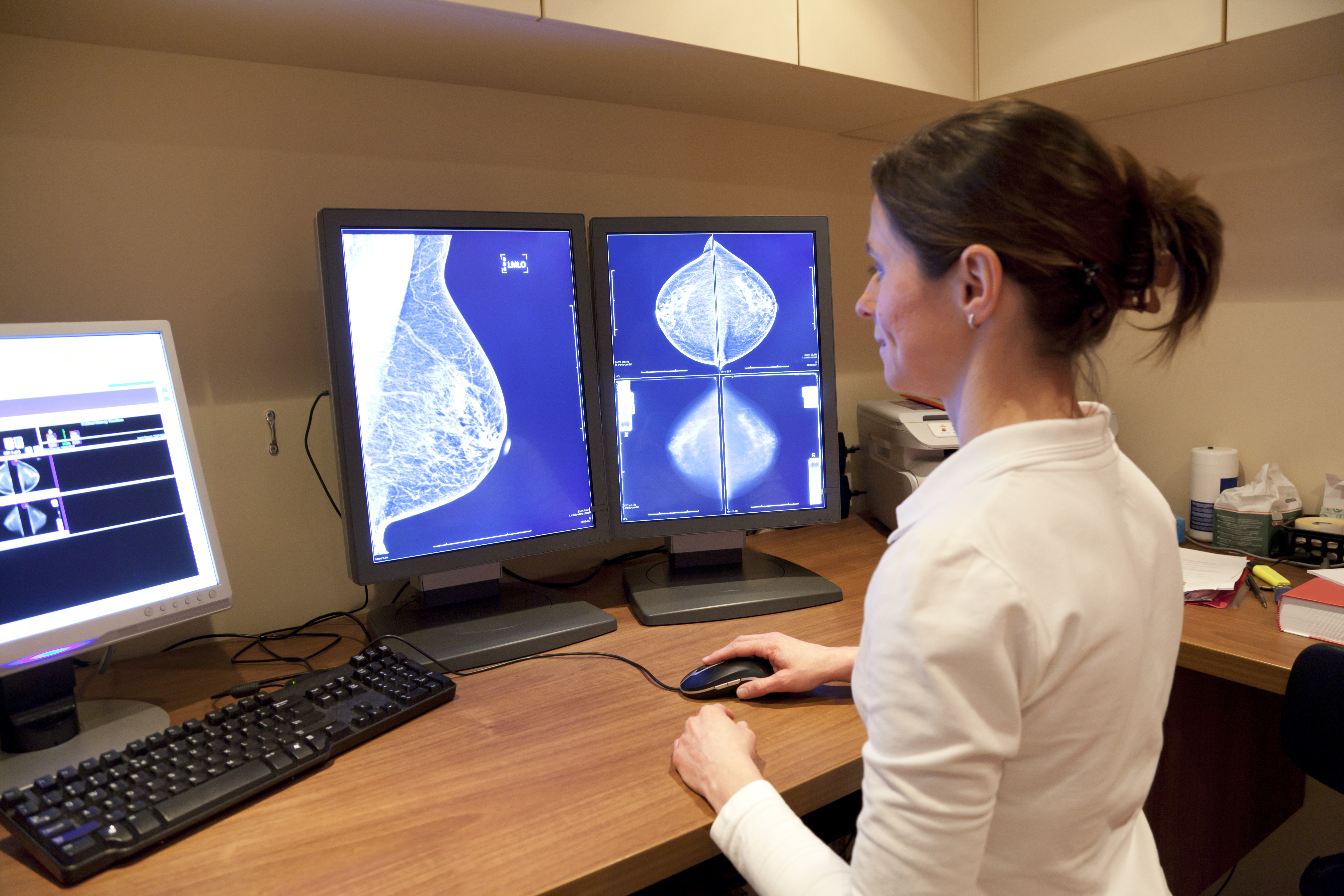
Mammography:
The mammography screening debate is complicated, and a more thorough discussion of the issues and research can be found in our response.
-- Screening mammography is testing performed in a healthy population to examine for presence of disease.
-- We have known for some time that screening mammography is not effective in women under age 40 because their dense breasts impede accurate results.[i]
-- Screening mammography for women over 40 or 50 years of age does not directly impact the young breast cancer survivors served by YSC.
-- We interpret the change in ACS' guidelines as a public admission that there is also no benefit to screening mammography between the ages of 40-44. Not only is there no benefit, but the risks outweigh the benefits enough for a change in recommendation to be warranted.
-- YSC concurs. We are not stating that screening mammography should be completely eliminated. We do believe, however, that women should be counseled about the risks and benefits of screening mammography, in consultation with their doctors, and make an individual decision that is best for them.
The above ACS recommendations address screening mammography only and do not impact the use of diagnostic mammography, a test performed because of a lump or other symptom that may suggest the presence of breast cancer. Diagnostic mammography is a vital tool. Women of any age with signs or symptoms of breast cancer should consult their doctors as soon as possible. In addition, screening mammography only addresses women at average risk of getting breast cancer in the general population. It is not for, and the research quoted does not address, screening in women at higher than average risk of being diagnosed with breast cancer (because of a BRCA 1 or 2 mutation, family history of breast cancer, or prior chest radiation), which includes screening residual breast tissue of breast cancer survivors of any age.
Clinical Breast Exams (CBEs):

-- The recommendation that a CBE, a physical exam to detect visible and palpable breast cancer by a medical professional, should not be performed was surprising.
-- In young women with breast cancer, 80% find the breast abnormality themselves[ii], suggesting that the cancer was palpable.
-- YSC has reviewed the data and did not find a strong basis for this recommendation. Therefore, YSC does not support this recommendation. When more clarifying evidence is received, we will review and reconsider the recommendation. We would welcome further explanation from ACS on their decision, as well as elucidation of the harms that could occur from CBEs and would outweigh the possible benefits.
-- Especially in populations without access to breast cancer screening, or who are too young to receive such screening, we are concerned about the recommendation to eliminate CBEs entirely.
What now?
-- Without other reliable screening options, we believe that CBEs should still be performed.
-- We recommend that all women are familiar with their breasts and aware of the signs and symptoms of breast cancer.
-- If you notice anything suspicious, you should see your primary care doctor or OB/GYN. It is important that you do not accept “You are too young for breast cancer” as an answer from a healthcare provider.
-- If you are a young woman at high risk for breast cancer, you should speak with a doctor about when you should begin breast screenings and which ones are best for you.
Whenever new screening guidelines come out, it can be confusing. Remember that these are guidelines for the general population and not women who are at higher risk. You can educate and empower yourself by reading YSC’s, “Breast Health and You: A Young Woman’s Guide.”
We would love to hear from you. What do you think of these new screening guidelines?
_______________
[i] Checka CM, Chun JE, Schnabel FR, Lee J, Toth H. The relationship of mammographic density and age: implications for breast cancer screening. AJR Am J Roentgenol. 2012; 198(3): W292-95. Doi:10.2214/AJR.10.6049.
[ii] Ruddy, K. et al., "Presentation of breast cancer in young women," Journal of Clinical Oncology 27:15S (2009).





